WHY THIS MATTERS IN BRIEF
AURA automates 200+ intricate IVF steps, dramatically scaling access to fertility care while reducing human error and costs.
Matthew Griffin is the World’s #1 Futurist Keynote Speaker and Global Advisor for the G7 and Fortune 500, specializing in exponential disruption across 100 countries. Book a Keynote or Advisory Session — Join 1M+ followers on YouTube and explore his 15-book Codex of the Future series.
In the posh Polanco neighbourhood of Mexico City, in a building tucked behind a Japanese restaurant, a sleek medical office upstairs had something new on display behind glass: a 17-foot-long, 4,500-pound robotic assembly line called the AURA. It’s an Artificial Intelligence (AI) powered fertility lab, the only mechanical system in the world that can achieve all the steps in making a human embryo – at least, the steps that can be done outside a woman’s body.
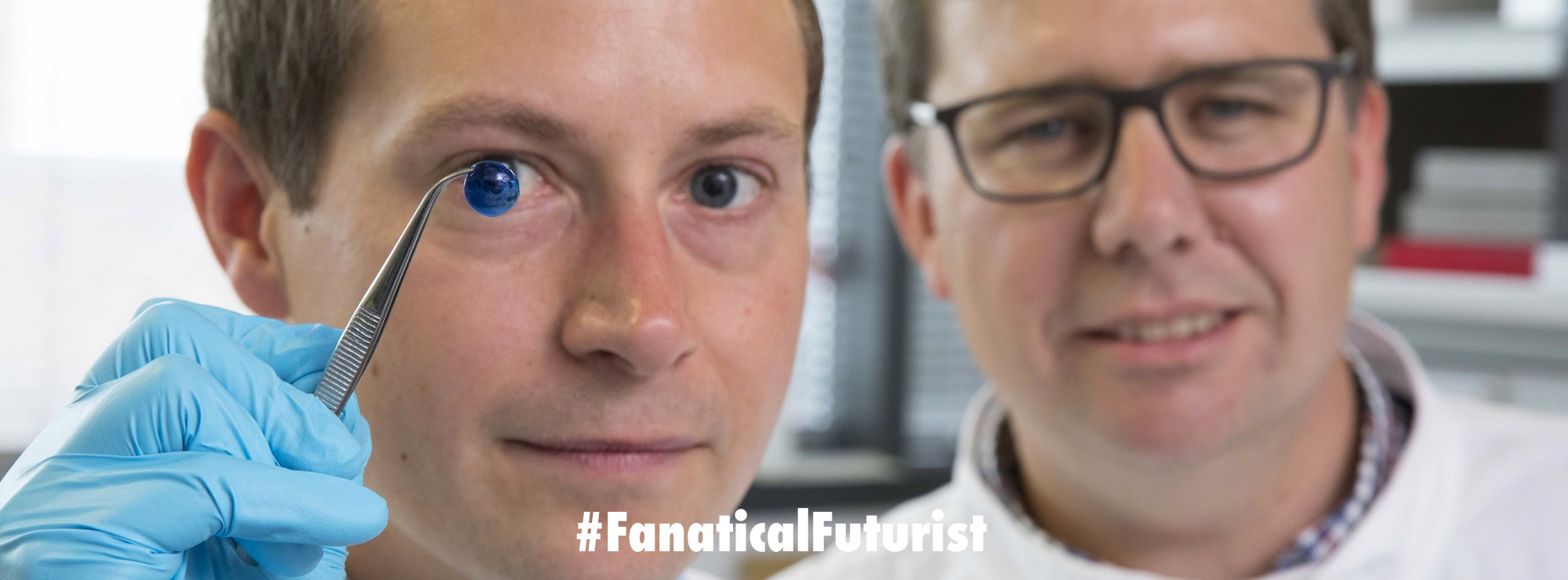
The AURA has six stations that use robot arms to manoeuvre pipettes and petri dishes. It tracks and selects swimming sperm, singles out good eggs and merges them to create the zygote. If everything goes well in AURA’s incubator, this zygote will become an embryo and then a blastocyst that can be transferred to a patient’s uterus, hopefully to grow into a baby.
The lab, created by New York-based startup Conceivable Life Sciences, stuns and collects sperm using the same ultraprecise robots that Meta and SpaceX use to manufacture hardware. Its algorithm for finding eggs in bloody follicular goop was adapted from one created by Chinese internet giant Baidu. Conceivable’s founders also drew inspiration from T-cell therapy, a form of cancer treatment that similarly involves taking cells out of a human, messing with them and putting them back in.
The medical office, Hope IVF, is owned by one of those founders. Patients, about 150 of whom are participating in a clinical trial to establish AURA’s efficacy, occasionally take selfies with the robots. When the machines are working on live human cells, the glass clouds up to keep private patient information out of public view, as technicians monitor the procedure from a room full of screens.
One bright morning in April, down the hall from the lab, there was a meeting of Conceivable’s founders: Chairman Joshua Abram, Chief Executive Officer Alan Murray and Chief Medical Officer Alejandro Chavez-Badiola, who’s also a doctor at the clinic, working with IVF patients the usual, hands-on way. They were discussing a recent parade of visitors from American and British clinic groups and research universities to see the AURA, weighing the pros and cons of selecting academics versus private-equity-owned clinic chains as launch partners next year – assuming, that is, the trial showed outcomes as good or better than the best conventional labs can produce.
Unlike in the US, fertility treatment is part of standard medical care in Mexico, and the country has been experiencing a boom in fertility tourism, making it relatively straightforward to start human trials there. The US is Conceivable’s main target, though. During their conversation, the founders said they’d spoken recently with White House officials about President Donald Trump’s executive order to make in vitro fertilization “drastically more affordable.” A representative for the administration offered to remove any regulatory “cobwebs,” Abram said.
Conceivable aims to expand access to fertility care by reducing the number of educated workers it requires and by raising the success rate for IVF, which produces live births only 37.5% of the time, according to 2022 data from the Centers for Disease Control and Prevention. The company doesn’t publish birth-rate numbers yet but does say that in single cycles its prototype robots can make embryos that turn into implantable blastocysts 51% of the time. That’s equivalent to what Hope IVF can do manually.
Right now, Conceivable’s founders said, fertility clinics aren’t meeting the demand from people who want children but haven’t been able to conceive on their own. Abram called the industry “concierge medicine for the rich.” Birth rates and sperm counts have been dropping worldwide, and people are choosing to become parents later in life. If these trends continue, according to the founders, demand for fertility treatment will only grow. In their view, fixing the gap isn’t a science problem so much as an engineering one. More precise and standardized IVF would also lessen the number of invasive, painful and expensive egg-generation cycles, dropping the cost and further increasing demand. The grand vision is that patients will one day be able to have their frozen eggs and sperm shipped to a “superlab” full of AURAs overseen by a single embryologist and two technicians. The robots could make thousands of embryos a day, compared with hundreds for that number of lab workers on their own.
There’s an unavoidably human part of this planned robot takeover: To win over investors and prospective patients, the founders, in concert with their peers in AI, need to evangelize the technology and make it sound inevitable. They’ve been hosting medical executives, hopping on the phone, even responding to skeptical commenters on their LinkedIn posts.
Conceivable’s critics argue that clinics, rather than patients, are more likely to reap the savings from automation, that it could result in errors being repeated at larger scale, and that sending gametes and embryos to and from a superlab could mean damage from transporting, thawing and freezing more than necessary.
Others have expressed more existential concerns, about further removing people from the process of creating life. The introduction of AI in IVF is “at the same time, medically promising and ethically disconcerting,” Sivan Tamir of the wrote in a 2022 paper. AI systems have the potential to make decisions in a way humans don’t totally understand, which could lead to “a general loss of human control over the procreation and continuity of the human species, as we know it.”
The likeliest path for Conceivable to win over investors, clinics and patients desperate for a child is to convince them that robots will be much better than humans at making humans. After a strategic chat with an executive from Merck, which supplied drugs for the trial, the founders met with Aike Ho, a partner with Acme Capital, for dinner. Ho wrote Conceivable’s first check in 2022 and a few years later decided with her wife, Camilla Hermann, to participate in the first human trials. The last time Ho saw these machines, they were prototypes in Guadalajara. Those prototypes made the couple’s embryos while the Conceivable team watched and celebrated “like it was a rocket launch,” Ho said.
One of the embryos was transferred to Hermann, who was on the Mexico City trip with Ho, 22 weeks pregnant. The ensuing months would be far from smooth – the pregnancy had to pull through medical uncertainty unrelated to the IVF procedure, and one of Conceivable’s founders became gravely ill. But in September, the AURA robots’ handiwork would result in the couple’s first child.
“People should be as excited about this as they were about the moon landing,” Ho said.
Ever since the first “test-tube baby” was born in the UK almost five decades ago, IVF has been politically and socially fraught, keeping it on the fringes of medicine. During the Bill Clinton administration, the US banned federal funding of any research involving the destruction of human embryos, which can happen during IVF; any innovation since then has happened mostly in other countries or with private money. More recently some states have conferred legal personhood on embryos, and the fertility industry has faced trust issues after some high-profile parentage mix-ups and a broad buy-up by private equity firms.
Still, with an estimated 1 in 6 people unable to conceive naturally and the average age of mothers climbing, consumer demand is soaring. The global fertility-services market is expected to grow from $64 billion in 2024 to $126 billion in 2029, according to Business Research Co. In the US, some major employers have started to help pay for egg retrievals and fertility treatments, and some states have begun requiring insurers to cover them in limited cases. Fertility has also become linked in the public consciousness with economic growth, especially among conservatives who prefer not to build the workforce through immigration. Some Billionaires such as Elon Musk talk about baby making alongside obsessions such as biohacking, longevity and the future of humankind.
A host of startups have emerged purporting to help Americans birth healthier babies, for example by training AI programs to advise patients on fertility treatment plans, to select the highest-quality sperm or to run genetic analyses of embryos. Labs in the US and the Netherlands are pursuing versions of artificial womb tech to keep premature babies alive – which when combined with AURA could actually see something like the clone breeding tanks that we see in Star Wars become real. There’s also early experimentation around growing egglike or spermlike cells from blood or skin cells using stem cells. Investors say this could pave a path to make a baby out of any cell in the body, a potential boon for infertile and same-sex couples, who could create one with both their DNA. In 2022 scientists said they’d grown mouse embryos synthetically, without the need for eggs or sperm at all.
For now, at least, assisted babymaking is the realm of modern fertility clinics, where success rates have plateaued in recent years and the process to create an embryo, even at the best labs, can be harsh on both egg and sperm.
The typical process is on display at Hope IVF’s manual lab in Mexico City, which sits in a room adjacent to the one with the robots. For starters, the sperm has to be separated from semen, which becomes toxic for sperm over time. To do this, a technician spins ejaculate in a centrifuge at 100 Gs, a level of force that can cause DNA to fragment if it goes for more than a few minutes. Next the millions of sperm are diluted in a solution and placed under a microscope. The embryologist picks one – often whichever is closest to the pipette tip and acting normally – and thwacks its tail with a needle to stop it from moving, then sucks it up.
As for the eggs, after follicular fluid has been removed from an ovary, an embryologist searches through the goop for one, then sucks it in and out of a pipette tube to generate friction that effectively washes off surrounding cells. The embryologist then punctures the egg’s external membrane – which isn’t easy, as the pressure from the needle briefly flattens the egg before the tip goes in – and places the sperm. It’s essentially single-cell surgery.
The lab transfers the zygote to an incubator to see if it starts growing into an embryo. If it does, it’s either prepared for immediate implantation or frozen. The latter sees the embryo submerged in a preservative – ethylene glycol, aka antifreeze, used even though it’s toxic, because no one has found an effective substitute – and plunged into liquid nitrogen for storage. Done improperly, this dunking can produce air bubbles that cause ice crystals to form; these can break the cell wall during the thaw, making the embryo unusable. And all of that is just for starters …
What is the AURA AI-powered fertility lab and how does it automate the IVF process? The AURA platform, developed by Conceivable Life Sciences, is the world’s first fully automated IVF lab that uses artificial intelligence and robot arms to achieve every step of human embryo creation outside the body. The system utilizes six integrated workstations to handle more than 200 manual steps, including sperm processing, egg discovery, and intracytoplasmic sperm injection (ICSI). By replacing variable manual processes with robotic precision and algorithmic guidance, AURA aims to standardize outcomes, lower costs, and expand fertility treatment access to millions of underserved patients globally.